Implications Of This Research
Implications for the NCSP and chlamydia coordinators
The NCSP should consider developing specific posters and leaflets promoting chlamydia screening that are suitable for the general practice waiting room. The posters need to be eye-catching for young people but not offensive to the elderly or those with young children. Leaflets need to be developed in different formats to suit different scenarios in the general practice setting. Credit card sized discrete leaflets would be more suited to receptions and waiting room areas, whereas longer leaflets are more suitable for clinicians to distribute as screening is offered. As staff suggested, in areas of high ethnicity the NCSP should consider leaflets in different languages and leaflets should inform young people how often they should be screened. Chlamydia coordinators need to promote and audit the use and display of chlamydia screening promotional materials more actively across all general practices registered with the chlamydia screening programme. Coordinators need to emphasise to practice staff that leaflets and posters need to be followed up with a verbal offer of screening opportunistically whenever a 15-24 year old visits the practice. All practice staff will need training on how to approach this.
In summary, the NCSP and coordinators of the service at PCT level should:
Make posters more suitable for a general practice setting
Make posters acceptable to elderly patients who may also view them
Implications for practices
How Chlamydia Is Treated
Chlamydia can usually be treated easily with antibiotics.
You may be given a course of doxycycline to take for a week or azithromycin to take once a day for 3 days.
If you have doxycycline, you should not have sex until you and your current sexual partner have finished treatment.
If you have azithromycin, you should wait 7 days after treatment before having sex .
It’s important that your current sexual partner and any other recent sexual partners you have had are also tested and treated to help stop the spread of the infection.
Under-25s who have chlamydia should be offered another test 3 to 6 months after being treated.
This is because young adults who test positive for chlamydia are at increased risk of catching it again.
Sexual health or genitourinary medicine clinics can help you contact your sexual partners.
Either you or the clinic can speak to them, or they can be sent a note advising them to get tested.
The note will not have your name on it, so your confidentiality will be protected.
Accuracy Of Screening Tests And Risk Assessment
The USPSTF found convincing evidence that clinicians could identify sexually active women at increased risk for chlamydial and gonococcal infections. It found adequate evidence that clinicians could identify sexually active men at increased risk for chlamydial and gonococcal infections. Seven new fair-quality studies with more than 93,000 participants were included in the analysis.34-39 In asymptomatic individuals, 3 studies with 71,636 participants that used a risk score to identify persons with chlamydial or gonococcal infections reported an area under the curve of 0.64 to 0.73.34-36 One study showed that age alone had accuracy similar to that for the use of more extensive risk criteria.39
Recommended Reading: Does A Zpack Cure Chlamydia
Complications From Chlamydia And Gonorrhea
Ruiz explained that for young women with asymptomatic infection, the effects of chlamydia and gonorrhea could be devastating.
They can cause a lot of damage to fallopian tubes. Years later, women who were asymptomatic and not treated show up with pelvic pain, and you find lots of scar tissue in the pelvis, said Ruiz.
Complications can also include:
- permanent damage to the reproductive system
- infertility
Key Interventions And Barriers To Receiving Care
Interventions to support high-quality information and care related to STIs include sex education programs, testing and treatment services, preventive technologies and vaccines, and supportive and dignified care. Unfortunately, young people face barriers in all of these areas.
Provide sexual health information. Young people deserve accurate and complete sex education in order to avoid STIs and mitigate their effects. Programs should provide students with accurate information about the prevention, transmission, symptoms and treatment of STIs. They should also equip students with skills to foster healthy relationships and express their sexual autonomy in a healthy way, such as by understanding consent and being able to advocate for condom use. The sexual health information provided should be age appropriate as well as responsive to and respectful of a range of cultural backgrounds, sexual orientations and gender identities.
Abstinence-only programs not only withhold important information from young people, but can actively harm them. This approach sends adolescents the message that sex outside of marriage is shameful or inherently dangerous, perpetuates gender stereotypes, ignores the experiences of LGBTQ youth and promotes a narrow view of an acceptable life course .23 Further, restricting sex education to a few topics contributes to misinformation and stigma that prevents adolescents and young people from seeking information and care related to STIs.
Read Also: How Do Men Get Tested For Chlamydia
Other Approaches To Prevention
The USPSTF has issued recommendations on screening for other STIs, including hepatitis B, genital herpes, HIV, and syphilis. The USPSTF has also issued recommendations on behavioral counseling for all sexually active adolescents and for adults who are at increased risk for STIs. These recommendations are available at .
Encouraging Others To Get Tested
Most of the never tested participants indicated that, if they happened to be CT positive, they would encourage sex partners to test, because they want to prevent transmission or would be concerned about their own and their partners health. Likewise, all tested participants had already, or would in the future personally encourage sex partners to test although they would find it difficult to do so. Some tested participants had themselves been encouraged by their sex partner or by someone within their trusted network to test for CT. A few tested participants and peers visited the clinic together for testing.
Interviewer: And why do you find it important that she is also tested?
Interviewee: Yeah, if I have it then she can also have it and imagine that she has it and then we do it again, and Ill have it again.
The last time that I had myself tested was because I heard via a former sex partner that he had got Chlamydia and that I should also be tested.
Despite anticipated negative reactions such as anger or shock, nevertested participants thought that their sex partners would go for a CT test once they had been encouraged by the participant to do so. This is in line with the positive experiences among tested participants where several sex partners they had talked to also got CT tested. Tested participants had not experienced negative reactions when encouraging others to test.
Read Also: Can Chlamydia Come Back On Its Own
Ncsp Support During Study Period
At registration with the NCSP, practices received a screening information pack and area-specific training. Over the study period, control and intervention practices continued to receive usual support from their local NCSP chlamydia coordinator who had an overall target chlamydia screening testing rate for 1624-year-olds in all NCSP venues across their area in 2009 of 25% and 2010 of 35% coordinators did not know practice study allocation. Usual support involved a single telephone contact or visit, availability to answer any queries by telephone, provision of testing kits when they were needed and partner notification.
Use Of Chlamydia Screening Posters In General Practices
Major themes
Use of posters
Two thirds of all screening practices said they had posters advertising chlamydia in their practices, which were either on the doors of their consulting rooms, in their waiting rooms or in patients’ lavatories.
We also had posters up around and also posters on our notice board outside and … it’s on our LED
There’s posters throughout the surgery isn’t there and in the passageways especially down by the nurses end. I don’t think the age group is on them. There was a poster up, but it has been taken down.
However, researchers observed that most posters displayed in general practices were aimed at elderly people or promoted immunisation very few had chlamydia posters in communal areas.
The difficulty with it, we tend to use the posters in the short term campaigns. We could do a campaign for an evening a month but then because of the wall space and everything we have to do. I mean we used to have lots of all sorts of posters, it was too messy and too much information to read.
Many staff thought posters caused offence. Several practices had to deal with complaints from older people about posters advertising chlamydia screening in the waiting room or lavatories and patients had either removed the poster themselves or had asked for it to be taken down.
We put up a poster on how to do it in the toilets that got taken down.
A few low screening practices reported other priorities for wall space and did not wish to prioritise one disease over another.
Read Also: How Many Pills For Chlamydia
Disclosure Of Ct Testing
All participants who had never tested reported that they would disclose CT testing and test results only to parents, good friends and sex partners whom they trusted, and from whom they expected a positive reaction . Likewise, all participants who had tested stated that they had only disclosed their test and its result to their trusted peers , receiving only positive reactions. Tested participants reported that it was self-evident to them that they inform sex partners. Tested participants received positive reactions from their trusted peers . Never tested and tested participants would not disclose to a broader network, because they anticipated shame and stigmatizing reactions, including gossiping and insulting language. For the never tested participants shame was associated with CT positivity and risky sexual behaviour. Due to the fact that no one disclosed their testing behaviour to peers outside the trusted network, experienced stigma from these people was avoided and tested participants reported no negative reactions. Similar responses were observed between men and women regarding their disclosure of test behaviour and results.
Chlamydia And Gonorrhea: Screening
Recommendations made by the USPSTF are independent of the U.S. government. They should not be construed as an official position of the Agency for Healthcare Research and Quality or the U.S. Department of Health and Human Services.
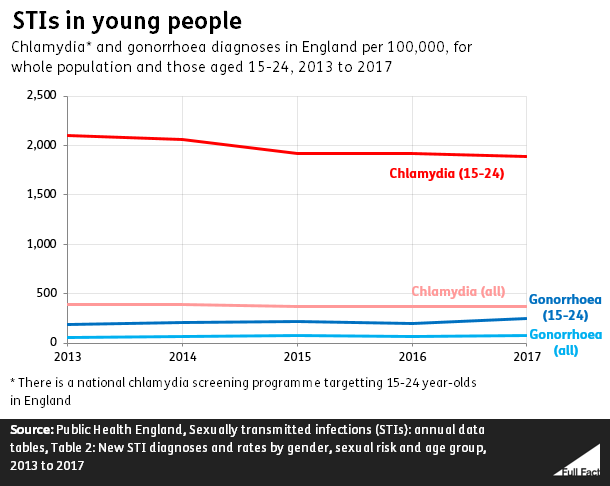
Chlamydia and gonorrhea are among the most common sexually transmitted infections in the US.1 Approximately 1.8 million cases of chlamydia and more than 600,000 cases of gonorrhea were reported to the Centers for Disease Control and Prevention in 2019. The rate of chlamydia infection among women was nearly double the rate among men . Gonorrhea infection was more prevalent in men than in women . Infection rates are highest among adolescents and young adults of both sexes. In 2019 almost two-thirds of all reported chlamydia infections, and in 2018 more than half of new gonococcal infections, were among persons aged 15 to 24 years.1,2
The US Preventive Services Task Force concludes with moderate certainty that screening for chlamydia in all sexually active women 24 years or younger and in women 25 years or older who are at increased risk for infection has moderate net benefit.
The USPSTF concludes with moderate certainty that screening for gonorrhea in all sexually active women 24 years or younger and in women 25 years or older who are at increased risk for infection has moderate net benefit.
Don’t Miss: Is It Hard To Get Rid Of Chlamydia
Summary Of Recommendations And Evidence
The USPSTF recommends screening for chlamydia in sexually active women aged 24 years or younger and in older women who are at increased risk for infection . B recommendation.
Screening for Chlamydia and Gonorrhea: Clinical Summary of the USPSTF Recommendation
Population
note: For a summary of the evidence systematically reviewed in making this recommendation, the full recommendation statement, and supporting documents, go to .
HIV = human immunodeficiency virus STI = sexually transmitted infection USPSTF = U.S. Preventive Services Task Force.
Screening for Chlamydia and Gonorrhea: Clinical Summary of the USPSTF Recommendation
Population
note: For a summary of the evidence systematically reviewed in making this recommendation, the full recommendation statement, and supporting documents, go to .
HIV = human immunodeficiency virus STI = sexually transmitted infection USPSTF = U.S. Preventive Services Task Force.
The USPSTF recommends screening for gonorrhea in sexually active women aged 24 years or younger and in older women who are at increased risk for infection. B recommendation.
See the Clinical Considerations section for a description of populations at increased risk for infection.
The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of screening for chlamydia and gonorrhea in men. I statement.
Number Of Chlamydia Infections Detected
The absolute numbers of Chlamydia infections detected in intervention practices increased from 2.1 prior to 2.5/1000 registered 1524-year-olds during the intervention, compared with 2.0 and 2.3 in control practices After allowing for the month of the first visit to the practice, and potential confounders including age, sex, PCT, month, deprivation quintile and baseline positive screen rates in each practice, the estimated rate ratio in the intervention practices was 1.4 times as great in the intervention practices compared with control practices . Positives detected remained for the 9months after the intervention ).
In fully engaged intervention practices, the number of chlamydia infections detected was 1.8 times as great as controls during the intervention period and 1.6 times as great in the 9months after than that seen in the control practices .
Read Also: Can You Be Exposed To Chlamydia And Not Get It
Prevalence Of Sexually Transmitted Infections
While women still account for the highest reported cases of STIs , men, in particular gay and bisexual men, saw greater increases in rates of syphilis, chlamydia, and gonorrhea in recent years. Syphilis infection rates nearly doubled among men from 2014 to 2018 .
| Table 1: Sexually Transmitted Infection Rates of Reported Cases, by Selected Characteristics, 2018Rate per 100,00 population | |
| 48.5 | 9.3 |
| NOTES: NR is Not Reported. Primary and secondary syphilis stages are the earliest stages of infection, reflect symptomatic disease, and are indicators of incident infection.SOURCE: Centers for Disease Control and Prevention , Sexually Transmitted Disease Surveillance 2018 CDC, Diagnoses of HIV Infection in the United States and Dependent Areas, 2018. |
Figure 1: Rates of sexually transmitted infections by sex from 2014 to 2018
Congenital syphilis rates increased 173% between 2014 and 2018, with the number of cases the highest they have been since 1995. The highest rates of congenital syphilis were in the South, West, and Southwest .
Figure 2: The highest rates of reported congenital syphilis are in the western and southern U.S.
STIs also have a disproportionate impact on young people, ages 15-24, who acquire half of all new STIs, despite only representing 25% of the sexually active population . Young people, ages 15-24, account for 60% of all reported cases of gonorrhea and chlamydia.
Figure 3: Young people bear a disproportionate burden of gonorrhea and chlamydia infections
Response To Public Comment
A draft version of this recommendation statement was posted for public comment on the USPSTF website from March 2 through March 29, 2021. Several comments expressed concern that the USPSTF found insufficient evidence to screen men and did not provide separate recommendations for specific high-risk populations. The USPSTF did not identify enough evidence to support that screening men for chlamydia and gonorrhea improves health outcomes by reducing infection complications or disease transmission or acquisition, including HIV. In the Research Needs and Gaps section, the USPSTF calls for more research on screening in men and other groups such as men who have sex with men the lesbian, gay, bisexual, transgender, queer/questioning community and racial and ethnic minorities. The USPSTF also clarified to whom the recommendation applies regarding sex and gender in the Practice Considerations section. Some comments requested that universal, rather than risk-based, screening be recommended for women 25 years or older. Based on available disease prevalence data and accuracy of risk assessment tools, the USPSTF found that younger age was a strong predictor of disease risk, which was clarified in the Practice Considerations section. Comments also asked for clarification on screening intervals. Given the lack of available evidence on optimal screening frequency, the USPSTF provides a reasonable approach for rescreening in the Practice Considerations section.
You May Like: Can You Catch Chlamydia Without Cheating
How Does Evidence Fit With Biological Understanding
Chlamydial and gonococcal infections are often asymptomatic in women. Untreated infections may progress to PID-related complications such as chronic pelvic pain, ectopic pregnancy, or infertility. Infections may also be transmitted to sex partners and newborn children. Accurate screening tests and effective antibiotic treatments are available for chlamydia and gonorrhea.
In men, gonococcal infections are more commonly symptomatic compared with women. Serious complications from infection are less common in men.
Studies on assessing risk and for whom screening may be most effective are a high priority.
The CDC recommends annual chlamydia and gonorrhea testing in all sexually active women younger than 25 years and in older women at increased risk of infection . It also recommends screening for both infections in pregnant women younger than 25 years and in older pregnant women at increased risk for infection during their first prenatal visit and again during their third trimester if risk remains high.16
The American Academy of Family Physicians follows the 2014 USPSTF chlamydia and gonorrhea screening recommendations.58 The American Academy of Pediatrics recommendations align with the CDC guidelines.59
Intervention Components Addressing Personal Attitudes Subjective Norms And Behavioural Controls
1) Changing personal attitudes:
Outcome beliefs, increasing belief in benefits of chlamydia screening tests:
-
Practice workshop demonstrating how common chlamydia is in 1624-year-olds, and the benefits of testing a usually asymptomatic pool of infections to reduce sequelae and onward transmission.
-
Feedback through newsletters to all staff and to practice champion, of testing activity and positivity may influence attitude towards the value of testing by demonstrating successful testing over time. For example, when increases in uptake and positives are observed, practice staff may feel that it is worth offering a chlamydia test.
Rewards of action increasing rewards they will receive by testing:
-
Develop testing targets based on a practice’s 1524-year-old population and consultations. Targets can act as a driver, so at the workshops explore the possibility of agreeing practice targets and milestones as a way of continually monitoring progress and keeping motivation high.
-
Feedback testing progress through monthly newsletters and at second practice visit/contact by chlamydia support worker.
-
Certificate of training attendance at practice workshop.
-
Certificate of personal development after doing on-line quiz.
2) Subjective norms
Normative beliefs :
Motivation to comply their willingness to test
3) Perceived behavioural control beliefs
Self-efficacy confidence in ability to test
External factors/control beliefs barriers or facilitators to testing at a practice level
Read Also: Can Strep Throat Antibiotics Cure Chlamydia